Do you have keratoconus? You’re not alone. If you have this eye condition, you know firsthand the challenges of experiencing distorted vision.
Patients with keratoconus used to have to wear hard, uncomfortable contact lenses or resort to a corneal transplant. But now, corneal collagen cross-linking, a revolutionary treatment, is transforming patients’ lives.
Keep reading to discover if having keratoconus means you should try corneal cross-linking!
What is Keratoconus?
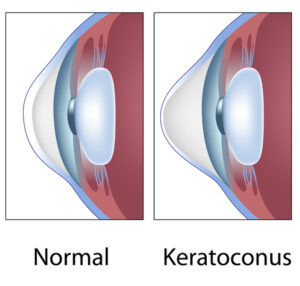
Keratoconus is an eye condition that affects the cornea. The cornea is the transparent outer layer of your eye.
Usually, the cornea is shaped like a dome. But when you have keratoconus, the cornea becomes thin, forming an irregular bulge and affecting your ability to see clearly.
People of any age can develop keratoconus. However, it’s typically first diagnosed in the early to late teens.
The rate of progression varies from person to person. It can progress especially quickly in children.
The exact cause of keratoconus is unknown. However, some factors are associated with an increased likelihood of having keratoconus.
Your risk of developing keratoconus increases with a known family history of the eye condition. You’re also more likely to develop keratoconus if you often rub your eyes or suffer from eye allergies.
Conditions that affect the body’s connective tissues, like Marfan syndrome, can also increase your risk of developing the eye condition.
How Does Keratoconus Affect Your Vision?

Keratoconus affects your vision due to the irregular shape of the cornea. The shape of the cornea is crucial for clear vision.
As light enters the eye, an evenly shaped cornea bends or refracts these rays onto the retina, creating focused images. When the cornea’s curvature is irregular, it cannot focus light correctly.
In most patients with keratoconus, the eye condition progresses slowly over many years. It typically begins to develop in late adolescence or early adulthood.
As it progresses, symptoms worsen. Blurring of vision may be mild at first. Keratoncous can also make straight lines appear wavy. Redness and light sensitivity are early symptoms of keratoconus too.
With time, more severe symptoms can occur. These include increased blurriness, nearsightedness, and astigmatism. As a result, everyday activities can become challenging.
It may also become uncomfortable or impossible to wear contact lenses. This is because they do not fit the irregular shape of the eye.
Keratoconus usually affects both eyes. However, they may exhibit different symptoms or severity of symptoms.
What is Corneal Cross-Linking?
Corneal cross-linking is an advanced treatment method for keratoconus. It can also be used to treat corneal ectatic disorders, including keratoconus.
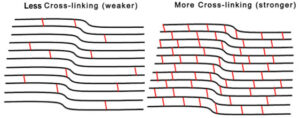
Corneal cross-linking uses a combination of ultraviolet light and vitamin B2 (riboflavin) to restabilize the cornea. The goal is to prevent the eye condition from worsening and stop further vision decline progression.
The procedure takes a few steps. First, you’ll have vitamin B2 eye drops applied. Next, your eye is exposed to a specific wavelength of ultraviolet light for about a half hour.
This light activates the riboflavin, creating new bonds between collagen fibers in the eye. Creating these new bonds strengthens the cornea and reduces further thinning to potentially improve vision over time. Collagen plays an essential role in maintaining the eye’s structure.
Corneal cross-linking is an outpatient procedure. After it’s over, you’ll return home to rest and recover.
Because of the numbing drops, discomfort is minimal. The recovery time is relatively short, about a week. Corneal cross-linking is a long-lasting treatment, with patients experiencing years of improvement due to it.
How Does Corneal Cross-Linking Treat Keratoconus?
Since its development and FDA approval, corneal cross-linking has become widely regarded as the most effective treatment for keratoconus. This is because, instead of merely addressing symptoms, it is intended to halt the progression of the eye condition.
Dell Laser Consultants has been at the forefront of corneal cross-linking since the beginning, as Dr. Dell was the first surgeon in Austin to offer this technology to patients. Corneal cross-linking strengthens the cornea by bonding collagen fibers in the eye.
This, in turn, flattens any bulging in the eye and helps prevent it from worsening. Corneal cross-linking has a very high success rate.
In most patients, thinning of the cornea stops entirely after this treatment. Studies of corneal cross-linking have also shown that it prevents vision loss in 95 percent of patients.
Plus, 60 to 70 percent of patients experience improved vision. This is because, by improving the shape of the cornea, the eye’s focusing ability can also improve.
Corneal cross-linking is intended to provide long-term effects. Evidence has shown no thinning or minimal thinning in patients a decade after treatment.
Who is Corneal Cross-Linking Best For?

Corneal cross-linking is an excellent option for those with keratoconus or corneal ectasia. Corneal cross-linking is commonly performed in patients with more advanced cases of keratoconus.
In the early stages of the eye condition, when symptoms are mild, glasses can be a sufficient solution for the time being. Your eye doctor may recommend corneal cross-linking as symptoms worsen to improve your vision.
Keratoconus tends to progress more rapidly in young people. Eye doctors often recommend performing corneal cross-linking early to preserve as much vision as possible for these individuals.
Your corneal thickness also affects whether you are a good candidate for this treatment. If your corneas are too thin, it may not be effective.
If you’re interested in corneal cross-linking, talk to your eye doctor. They can help determine whether this is a suitable treatment for you.
Are you considering corneal cross-linking? Learn more about corneal cross-linking and if it could be a good way to treat your keratoconus by requesting an appointment at Dell Laser Consultants in Austin, TX. Don’t let impaired vision stand in the way of living your best life!